Keratoconus
Keratoconus, the cornea, which is the outermost transparent layer of the eye and the area where the light coming from outside is first refracted, tends to progressmyopia and astigmatism It is an eye disease in which the structure deteriorates, becomes thinner and bulges forward. It mostly affects people between the ages of 10 and 25 worldwide. Keratoconus usually progresses between the ages of 20 and 40. This progress slows down after the age of 40. The disease is often noticed in the 20s.
Keratoconus, which is among the corneal diseases, usually affects one eye more than the other. Genetic factors mostly play a role in the emergence of the disease. Therefore, regular ophthalmologist check-ups are of great importance for individuals with a family health history of this disease. Keratoconus symptoms are usually noticed late. The progression of the disease occurs slowly, over a long period of time. Vision gradually decreases over time. While it may occur in both eyes, it may progress less in one eye than the other. There are various methods for treatment that are multi-stage and vary depending on the level of the disease. With early diagnosis, an easier treatment opportunity emerges. If the disease is left untreated or treated late, there is a risk of resulting in permanent vision loss.
SUBJECT TITLES
What is Keratoconus?
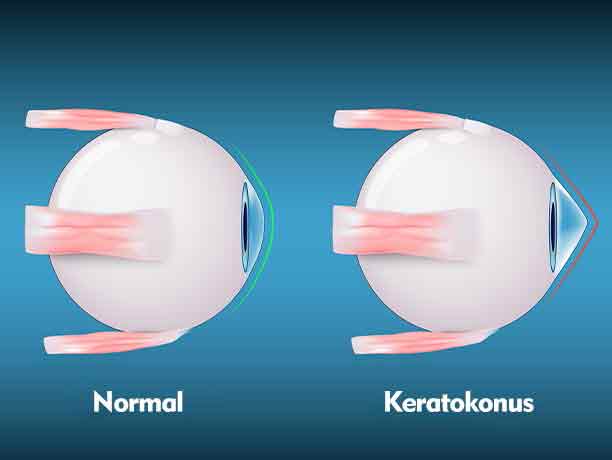
Keratoconus is an eye disease that occurs as a result of the cornea thinning and tapering forward, causing various vision defects. The disease occurs in the cornea, the most anterior segment of the eye. The cornea is the area where light first enters the eye. It helps refract the light coming into the eye from outside and focus it on the retina. As the cornea tapers forward and becomes thinner after keratoconus, the light coming into our eyes from outside is not focused properly in the visual field on the retina. As a result of this situation, vision loss occurs.
Although the cause of keratoconus is not fully known, some scientific studies reveal that genetic factors play a major role in the development of the disease. Therefore, people with a family history of keratoconus should have regular medical check-ups.
In addition, imbalances in the enzymes in the cornea are observed during the development of the disease. As a result, the cornea becomes more vulnerable to oxidative damage and tapers forward with the thinning of its surface.
What are the Risk Factors?
- Some genetic diseases such as Down Syndrome, Osteogenesis Imperfecta, Marfan Syndrome.
- Hap fever during childhood and constant eye rubbing are risk factors for triggering keratoconus disease in people with sensitive corneal structure.< /li>
- The use of contact lenses that are not compatible with the eye can trigger the disease by creating a degenerative effect on the cornea.
- Congenital eye anomaly,
- Too much exposure to unprotected UV rays in daily life throughout life,
- Low level of collagen in the cornea,
- Factors such as night blindness (chicken black disease),
- Chronic eye irritation,
are among the risk factors for keratoconus.
What are the symptoms of Keratoconus?
Among the symptoms of the disease, observed in the first stage, is the change in the shape of the cornea and the development of irregular myopia and astigmatism in patients. Astigmatism occurs when the cornea protrudes from its smooth and round shape to a cone shape, and myopia occurs when the front side of this protrusion gradually widens.
The progression of these symptoms usually takes years. In some cases, the course may suddenly accelerate and worsen. If the progress is not monitored and the necessary measures are not taken in time, excessive corneal thinning and edema may occur.

Keratoconus symptoms are as follows:
- Slight blurring of vision in the initial stages and serious blurring in advanced stages,
- Fluctuations and curvatures in the appearance of straight lines,
- Frequent improvements in eye numbers,
- Dazzle and seeing halos on illuminated objects,
- Double vision and image multiplication when looking with one eye,
- Night impaired vision and difficulty in driving at night,
- Eye allergy or itching,
- Symptoms such as the contact lens used in the past not fitting into the eye properly, frequent change of glasses and blurred vision after a while despite using glasses, are common symptoms.
How to Treat Keratoconus?
Keratoconus treatment is a multi-stage treatment. Although early diagnosis is important in treatment, there may be different treatment options for the initial and advanced stages of the disease.
In the first stage of the treatment process, the patient is explained how the treatment process will be and what the patient should do during this process. Thus, risk factors are minimized. Depending on the degree of the patient, glasses or soft contact lenses may be prescribed to the patient.
Scleral or rigid gas permeable lenses can be used in the treatment for the early stage. These lenses improve vision, but they cannot definitively stop the progression of the disease. These lenses need to be used constantly and can slow down the progression of the disease as long as they are used continuously. The disease generally progresses more rapidly after its use is discontinued.
Corneal Cross-linking treatment and hybrid treatment are applied to stop the progression of the disease and improve the quality of vision.
If the disease is detected late or no treatment is required. In very advanced patients who do not respond, the need for corneal transplantation may arise.
Hybrid Treatment Method
Another method used in treatment is hybrid treatment. Hybrid therapy was developed by New York University. In this treatment, the irregularities on the corneal surface are eliminated with a no touch laser and the cornea is strengthened with vitamin B2 + ultraviolet light therapy applied in the same session. Thus, the progression of the disease is stopped. The person can receive both Cross Linking, which helps stop the progression of the disease, and vision-improving laser treatment in the same session.
